Picture Credit: Wikivet
Interdigital dermatitis is a condition that leads to lameness in sheep and goats and is often a predisposing factor to footrot. It is sometimes referred to as Benign Footrot. It is a mixed bacterial infection however, Dichelobacter nodosus has been recognized as the major cause of this condition. Other causal factors of this disease include wet weather, muddy pens, and damp pastures. Diagnosis is based on clinical signs and laboratory testing.
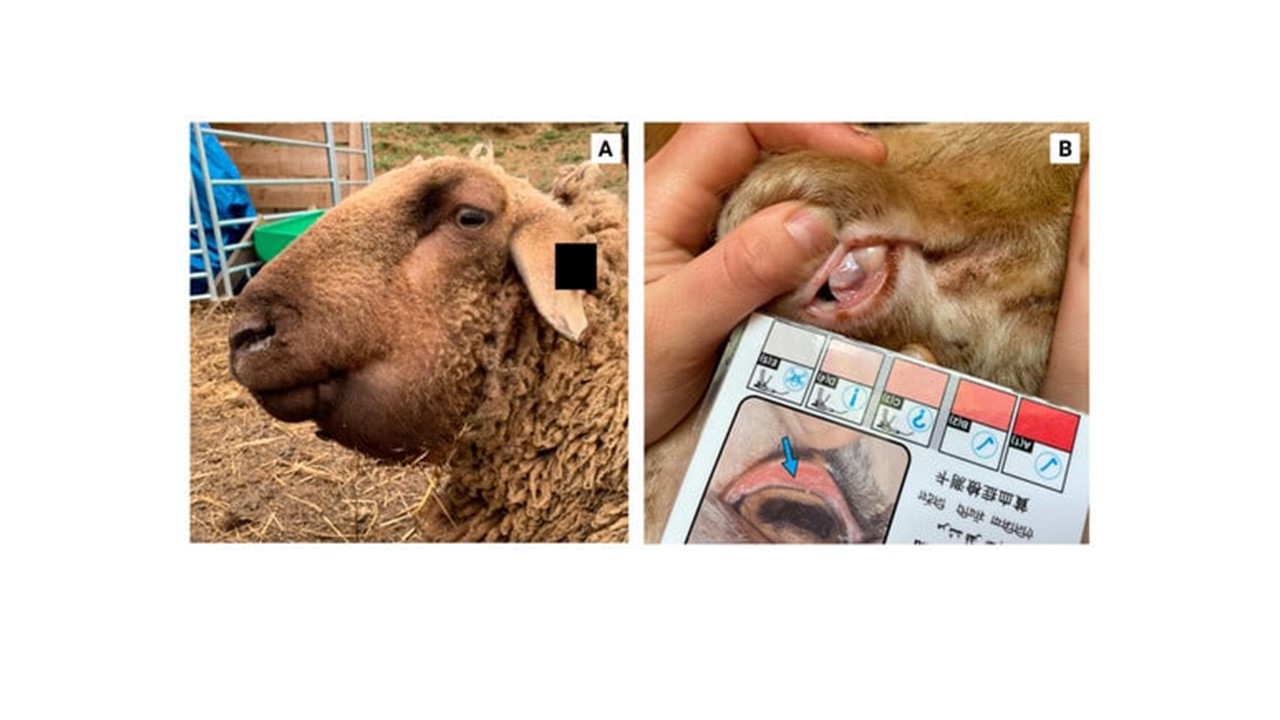
CLINICAL SIGNS
The interdigital skin is red and swollen and may be seen as covered with a thin layer of white exudate. The hoof capsule may be shed in very severe cases. Chronic infections can lead to lameness and formation of misshapen hooves.
TREATMENT, PREVENTION AND CONTROL
The use of topical aerosol antibiotic sprays have proven to be very effective. In farm herds where large numbers have been affected, the whole flock can be treated with 10% Zinc Sulphate solution or 3% formalin in a footbath. High concentrations of formalin greater than 5% can cause irritations. Sheep must be made to stand in a dry area for the formalin or the zinc sulphate to dry on the feet. Footbaths must be repeated (after a week or two). There is no need to attempt foot trimming.